Supporting Autistic Individuals Through Pregnancy
Introduction
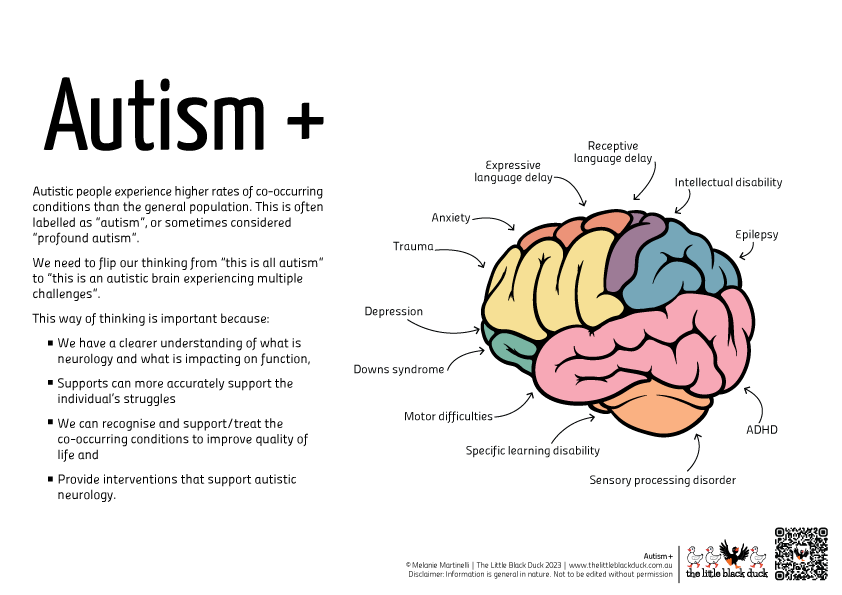
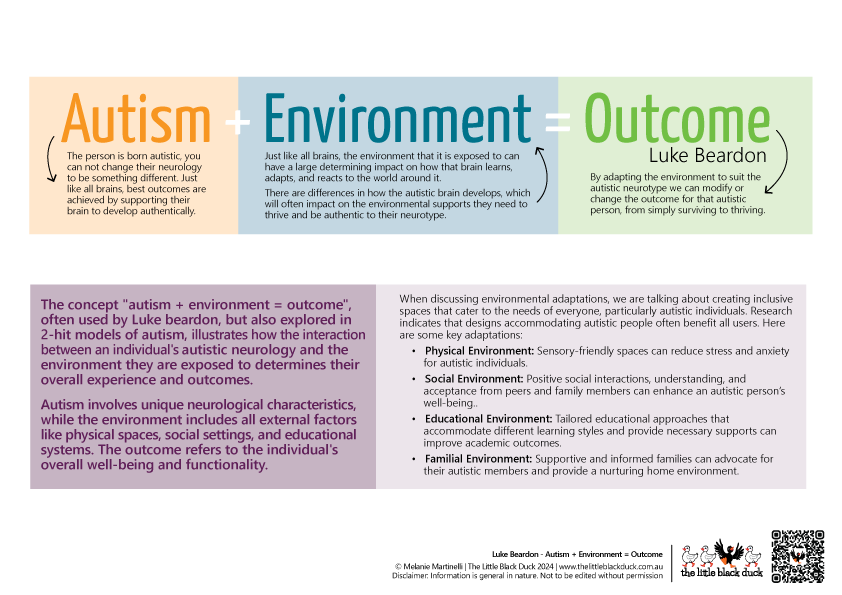
Pregnancy is a significant period of physical, emotional, and social transformation. For autistic individuals, these changes often interact uniquely with sensory processing differences, communication styles, and co-occurring conditions, creating distinct challenges that are underrepresented in research. While pregnancy has long been explored through the lens of neurotypical experiences, recent literature highlights that autistic people frequently encounter sensory sensitivities, heightened anxiety, and barriers to healthcare access during this period (Hampton et al., 2021; Ferrara et al., 2023).
Research also underscores that the prevailing medical model of maternity care often fails to accommodate neurodiverse needs, contributing to negative experiences and poorer health outcomes. Sensory triggers, such as the bright lights and loud sounds common in clinical environments, can exacerbate sensory overload during medical appointments and childbirth (Wilson et al., 2022
PubMed). Furthermore, communication barriers, coupled with healthcare providers’ lack of autism-specific training, often hinder effective care delivery (Crane et al., 2021).
The purpose of this assignment is to explore how maternity services can be made more inclusive, identifying key adaptations to better support autistic individuals during pregnancy, childbirth, and the postpartum period. By integrating contemporary research, this report aims to provide actionable recommendations to enhance the experiences of autistic parents.

Challenges in Pregnancy for Autistic Individuals
Pregnancy introduces a range of physical, sensory, and emotional experiences that interact uniquely with autistic neurology. For many autistic individuals, the process of navigating pregnancy involves heightened sensory sensitivities, amplified responses to sound, light, touch, and smell, and difficulties adapting to the rapidly changing physical and social demands (Hampton et al., 2022; Ferrara et al., 2023).
Difficulties with Transitions and Change
Pregnancy often requires frequent transitions—shifts in physical abilities, healthcare routines, and social roles—that can be particularly challenging for autistic individuals. Autistic neurology is characterised by a preference for predictability and routine, which may conflict with the unpredictable nature of pregnancy. This can lead to increased anxiety and difficulty coping with new or unexpected demands (Hampton et al., 2022). For example, many autistic individuals report distress when faced with changing healthcare providers or unexpected alterations in care plans, such as an emergency caesarean delivery or unanticipated medical interventions (Wilson et al., 2022
PubMed).
Healthcare systems often exacerbate these challenges, as they are rarely designed to accommodate the need for gradual, well-communicated transitions. Research highlights the importance of providing clear, step-by-step explanations and minimising last-minute changes to reduce stress and sensory overload (Crane et al., 2021).
Higher Rates of Pregnancy-Related Conditions
Autistic individuals appear to experience pregnancy-related complications at higher rates than their neurotypical peers, which further compounds their challenges. Studies suggest an increased prevalence of conditions such as gestational diabetes, hyperemesis gravidarum, and pelvic girdle pain in autistic individuals (Hampton et al., 2022). Sensory sensitivities often intensify the discomfort associated with these conditions; for instance, nausea linked to hyperemesis gravidarum may be exacerbated by heightened olfactory sensitivity.
Additionally, differences in proprioception and connective tissue disorders, which are more prevalent in the autistic population, may increase the risk of pelvic and joint pain during pregnancy (Ferrara et al., 2023). Despite these elevated risks, autistic individuals frequently report that their symptoms are dismissed or inadequately addressed in maternity care, contributing to feelings of neglect and frustration.
Mental Health and Emotional Well-Being
Mental health challenges are a persistent concern during pregnancy, with autistic individuals being at a heightened risk for anxiety, depression, and prenatal or postnatal depression. The stress of managing pregnancy-related conditions alongside systemic barriers to care amplifies this risk (Ferrara et al., 2023). Social isolation, which is commonly reported by autistic people, further exacerbates feelings of vulnerability during pregnancy (Hampton et al., 2021).
Efforts to address these challenges must involve not only individualised support but also systemic changes in healthcare environments. Providing sensory-friendly adjustments, offering predictable care pathways, and improving provider training are vital to creating a more inclusive experience for autistic individuals navigating pregnancy.
Stigma, Masking, and Pregnancy

Stigma in Healthcare and Society
Despite growing awareness of autism, stigma continues to pose significant barriers for autistic individuals, particularly during pregnancy. Stereotypes that portray autism as a primarily male condition, or misunderstandings about how it manifests in females and transgender individuals, often result in underdiagnosis, misdiagnosis, or dismissive attitudes from healthcare providers (Ferrara et al., 2023). This stigma is further compounded for autistic individuals navigating pregnancy, where societal expectations around maternal identity and behaviour often clash with their lived experiences.
For transgender individuals, these challenges are magnified by additional layers of discrimination and systemic bias in healthcare. Misgendering, lack of culturally competent care, and inadequate accommodations for sensory and communication needs create a compounded burden for those seeking pregnancy-related care. Studies highlight that the intersection of autism and gender diversity frequently leaves individuals feeling marginalised and unsupported during their maternity care journey (Wilson et al., 2022
PubMed).
Stigma also manifests in healthcare professionals’ assumptions about parenting abilities. Autistic individuals often report that their capacity to parent is questioned, with some facing inappropriate referrals to child protection services due to a lack of understanding of autism-related behaviours (Hampton et al., 2021). This fear of being judged or having their parenting scrutinised discourages many autistic parents from disclosing their diagnosis or seeking help when needed, creating additional barriers to accessing effective support.
The Role of Masking
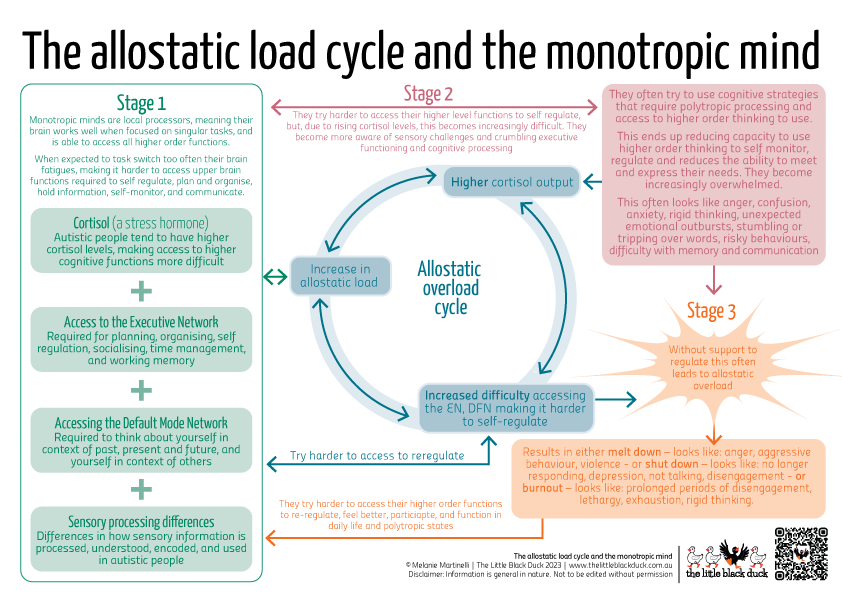
Masking, or the conscious or unconscious suppression of autistic traits to conform to societal norms, is a well-documented phenomenon among autistic individuals. While masking may help individuals navigate social interactions, it comes at a significant cost to mental and physical health. During pregnancy, the pressure to mask can intensify as autistic individuals attempt to meet societal expectations of maternal behaviour or suppress sensory sensitivities to avoid judgement (Hampton et al., 2022).
Masking often leads to increased fatigue, stress, and emotional burnout, particularly when compounded by the physical and emotional demands of pregnancy. Furthermore, masking behaviours can obscure an individual’s needs, leading healthcare providers to underestimate the level of support required (Crane et al., 2021).
For transgender autistic individuals, masking can also involve suppressing both autistic traits and gender identity to avoid discrimination or misgendering. This dual-layered masking increases the risk of negative mental health outcomes, including heightened anxiety and depression during pregnancy (Wilson et al., 2022
PubMed).
Reducing Stigma and Supporting Authenticity
Addressing stigma and the need for masking requires systemic changes within healthcare and society. Autism training for maternity care providers should include education on the diverse presentations of autism, particularly in females and transgender individuals, and the potential harms of masking. Creating environments where autistic individuals feel safe to disclose their diagnosis and express their needs without fear of judgement is essential.
Additionally, adopting a neuro-affirming approach that celebrates diverse parenting styles and recognises the unique strengths of autistic parents can help to dismantle stigma. For transgender individuals, this also means providing culturally competent care that affirms their gender identity and ensures their maternity journey is respectful and inclusive.
Communication and Service Adaptations
Clear and consistent communication is essential in maternity care, yet autistic individuals often encounter barriers in their interactions with healthcare providers. Research highlights that healthcare professionals frequently lack training in autism, leading to misunderstandings and unmet needs (Hampton et al., 2021; Ferrara et al., 2023). Autistic people often express a preference for direct, unambiguous communication, coupled with visual aids or written information to support verbal instructions (Wilson et al., 2022
PubMed).
Providing Detailed Explanations
Taking the time to provide detailed explanations about what is happening during appointments or procedures can significantly lower distress for autistic individuals. Many experience heightened anxiety when faced with uncertainty or abrupt transitions, making it essential for healthcare providers to explain each step thoroughly and allow time for questions or processing. For instance, clearly outlining the purpose of a medical procedure, the expected sensations, and the anticipated duration can help autistic patients feel more prepared and in control during their care (Hampton et al., 2022).
Additionally, ensuring that explanations are concise and free from ambiguous or “fluffy” language reduces cognitive load and aids comprehension, particularly for individuals who may struggle with processing verbal information during high-stress situations (Crane et al., 2021).
Mindfulness of Sensory Needs
Appointments in clinical settings can be highly confronting due to sensory triggers such as bright lights, noisy equipment, or crowded waiting rooms. Being mindful of these sensory needs and making simple accommodations can greatly improve the experience for autistic individuals. Strategies such as dimming lights, reducing noise, or offering quieter appointment times can help create a less overwhelming environment. Providing sensory tools, such as noise-cancelling headphones or weighted blankets, further supports patients in managing sensory challenges during care (Wilson et al., 2022
PubMed).
Interpreting Affect and Behaviour
It is important to note that an autistic person’s outward affect does not always reflect their inner experience. In situations of sensory or emotional overwhelm, individuals may appear calm or even engaged but may, in fact, be shutting down to manage the overload. This can lead healthcare providers to mistakenly assume the person understands what is being communicated or is coping well with the situation. Adopting a communication style that prioritises checking for understanding and offering opportunities to revisit or clarify information can help ensure the patient’s needs are fully met (Hampton et al., 2021).
Balancing Predictability and Flexibility
Establishing predictable routines for appointments, including consistent schedules and familiar faces, fosters a sense of safety and reduces anxiety. At the same time, allowing flexibility to adjust care based on individual sensory and communication needs is crucial. For example, offering longer appointment times ensures that patients have adequate time to process information, ask questions, and acclimate to their surroundings without feeling rushed (Hampton et al., 2022).
Disclosure and Trust
Disclosing an autism diagnosis is a complex decision for many autistic individuals. While disclosure can lead to necessary accommodations, such as sensory-friendly adjustments, it is also fraught with risks of stigma and inadequate understanding from providers (Hampton et al., 2022). Establishing trust through compassionate communication and a willingness to adapt care to individual needs can encourage disclosure, enabling healthcare providers to deliver more tailored and effective support.Recommendations for Improving Maternity Care
To ensure autistic individuals experience safe, supportive, and inclusive maternity care, healthcare providers must adopt neuro-affirming practices that address sensory, communication, and emotional needs. The following recommendations draw on contemporary research and aim to create a more accessible maternity care model.
1. Autism-Specific Training for Healthcare Providers
Healthcare providers often lack a foundational understanding of autism, particularly its presentation in adults and gender-diverse individuals (Ferrara et al., 2023). Mandatory autism-specific training should be integrated into maternity care curricula, covering sensory sensitivities, communication preferences, and the potential for masking behaviours. This training should also emphasise the importance of recognising diverse presentations of autism, particularly in females and transgender individuals, whose experiences may differ from widely held stereotypes.
2. Creating Sensory-Friendly Environments
Sensory overload is a common challenge for autistic individuals in clinical settings. Maternity care providers should adopt sensory-friendly practices, such as dimming lights, reducing noise, and allowing patients to bring sensory tools (e.g., headphones, fidget items). Offering quieter appointment slots or home visits can further minimise sensory distress (Wilson et al., 2022
PubMed).
In labour and delivery settings, options for personalised birthing plans that incorporate sensory needs—such as soft lighting, limited staff in the room, and sensory breaks—should be readily available. Providing recovery spaces with low sensory input post-birth can also aid in emotional regulation and facilitate bonding with the newborn (Hampton et al., 2022).
3. Enhancing Communication and Information Delivery
Healthcare providers should prioritise clear, direct, and patient-centred communication. Written summaries of appointments, visual aids, and step-by-step explanations of procedures help reduce cognitive load and ensure understanding. Allowing extra time for appointments and offering opportunities for questions or clarification are crucial for building trust and reducing anxiety (Crane et al., 2021).
Providers should also check for understanding without relying solely on outward affect, recognising that calm demeanours may mask internal distress. This approach ensures that care aligns with the patient’s needs rather than assumptions about their experiences (Hampton et al., 2021).
4. Building Continuity of Care
Continuity of care is essential for reducing stress associated with frequent transitions and unfamiliar providers. Assigning a consistent care team throughout pregnancy, labour, and postpartum improves trust and ensures that healthcare professionals are familiar with the individual’s sensory, communication, and medical needs (Wilson et al., 2022
PubMed). When continuity cannot be maintained, comprehensive care plans and effective handovers between providers become critical to maintaining quality care.
5. Supporting Emotional and Mental Well-Being
Given the increased risk of anxiety, depression, and prenatal or postnatal depression among autistic individuals, maternity services must integrate mental health support as a core component of care. Providing access to autism-informed counselling, peer support groups, and postnatal follow-ups focused on emotional well-being can significantly improve outcomes (Ferrara et al., 2023).
Creating peer-led support networks, particularly for autistic parents, fosters a sense of community and reduces isolation. These groups can also provide practical advice on managing sensory challenges and navigating maternity services (Hampton et al., 2022).
6. Affirming Gender and Neurodiversity
Inclusive maternity care must recognise and affirm the intersecting identities of autistic individuals, particularly for transgender and nonbinary parents. This includes respecting self-identified pronouns, providing gender-inclusive language in maternity settings, and offering specialised support for the unique challenges faced by transgender individuals during pregnancy (Wilson et al., 2022
PubMed).
Additionally, healthcare providers should adopt a neuro-affirming approach that values autistic traits and celebrates diverse parenting styles. Reframing autism-related behaviours as strengths rather than deficits contributes to a more positive and empowering maternity care experience.
Intersectionality: Autism, Gender, and Cultural Diversity in Pregnancy

The experience of pregnancy for autistic individuals is shaped not only by their neurodivergence but also by the interplay of gender identity, cultural context, and socioeconomic status. Understanding these intersections is critical to providing inclusive, tailored maternity care.
Cultural Variations and Perceptions of Autism in Pregnancy
Cultural beliefs about pregnancy and parenting can significantly influence the experience of autistic individuals. In some cultures, pregnancy is accompanied by strict social norms and expectations that may conflict with an autistic individual’s needs or sensory preferences. Furthermore, cultural stigma surrounding autism often creates additional barriers to accessing care. For example, in cultures where autism is poorly understood or highly stigmatised, autistic individuals may feel pressured to mask their traits to conform to societal expectations (Ferrara et al., 2023).
Language barriers, combined with sensory challenges and differences in communication styles, can further marginalise autistic individuals from culturally and linguistically diverse backgrounds. To bridge these gaps, healthcare providers must adopt culturally sensitive practices that respect diverse beliefs while prioritising the individual’s needs.
Experiences of Transgender and Nonbinary Autistic Individuals
Pregnancy is often framed within cisnormative assumptions, which can alienate transgender and nonbinary autistic individuals. These individuals frequently face dual layers of discrimination—one for their gender identity and another for their neurodivergence. Misgendering, the use of gendered language in maternity settings, and inadequate training in trans-affirming care exacerbate stress and isolation (Wilson et al., 2022
PubMed).
For transgender autistic individuals, masking behaviours may involve suppressing both gender identity and autistic traits, leading to heightened emotional and physical exhaustion during pregnancy. This dual burden underscores the need for inclusive practices, such as offering gender-neutral language, respecting self-identified pronouns, and creating safe spaces for open communication about sensory and medical needs.
Healthcare providers should also be prepared to address the unique medical needs of transgender individuals during pregnancy, including hormonal considerations and mental health support tailored to their intersecting identities.
Socioeconomic Disparities in Access to Care
Socioeconomic status significantly impacts an individual’s ability to access autism-informed maternity care. Autistic individuals from lower-income backgrounds often encounter financial barriers, limited healthcare options, and inadequate social support systems, which amplify the challenges of navigating pregnancy (Ferrara et al., 2023).
Additionally, autistic individuals who rely on public healthcare systems may face longer wait times, limited continuity of care, and fewer sensory-friendly accommodations. Policies that prioritise equitable access to autism-informed care, regardless of socioeconomic status, are essential to mitigating these disparities.
Toward Intersectional Maternity Care
Addressing the intersections of autism, gender, and cultural diversity requires a holistic and inclusive approach. Healthcare providers should adopt intersectional frameworks that recognise and affirm the unique experiences of each individual. This includes:
- Cultural Competency Training: Educating providers on the diverse cultural and gendered experiences of autistic individuals to reduce biases and improve care.
- Flexible Care Models: Designing maternity services that accommodate varying cultural, linguistic, and financial needs.
- Advocacy and Policy Change: Supporting systemic reforms that ensure equal access to neuro- and gender-affirming care for all autistic individuals.
By acknowledging and addressing these intersecting factors, maternity care can become a safe and empowering experience for autistic individuals, regardless of their background or identity.
Autistic Strengths and Positive Experiences in Pregnancy
While much of the literature focuses on the challenges faced by autistic individuals during pregnancy, it is equally important to highlight the unique strengths and positive experiences that neurodivergent individuals bring to this life stage. By reframing traits often viewed as deficits, maternity care can foster an empowering and supportive environment that celebrates diversity.

Systemising and Planning Skills
Autistic individuals often excel in systemising and planning, traits that can be invaluable during pregnancy and parenting. Many autistic parents report using their organisational skills to prepare for childbirth and parenthood, creating detailed birth plans, researching extensively about pregnancy, and devising strategies to manage potential sensory challenges during labour (Wilson et al., 2022
PubMed; Dugdale et al., 2021). These traits contribute to creating predictable, stable environments that benefit both the parent and child.
Research also highlights how autistic parents adapt these skills to manage daily caregiving demands, demonstrating resilience and innovation in the face of systemic challenges.
Unique Sensory Bonding with the Baby
Sensory sensitivities, often framed as challenges, can enhance the bonding experience between an autistic parent and their baby. Autistic parents may derive profound joy from observing subtle cues in their baby’s expressions, sounds, and movements, forming an intense connection that fosters a deep understanding of the child’s needs (Hampton et al., 2022; Dugdale et al., 2021). This sensory attunement contributes to a nurturing and empathetic parenting style, particularly when raising neurodiverse children.
One study noted that many autistic parents felt a strong affinity with their child’s sensory experiences, deepening their connection and fostering a shared understanding within the family dynamic.
Attention to Detail and Routines
Many autistic individuals thrive on routine and attention to detail, traits that can be advantageous during the early stages of parenting. These traits translate into consistent caregiving practices, such as feeding schedules, sleep routines, and monitoring developmental milestones, which create a sense of stability for the child (Ferrara et al., 2023; Garcia-Molina & Cortés-Calvo, 2024).
For autistic parents, the ability to identify and respond to small changes in their child’s behaviour or environment is a significant strength, enabling proactive and responsive caregiving.
Resilience and Advocacy
The lived experiences of navigating systems that often overlook neurodiverse needs equip autistic individuals with resilience and strong self-advocacy skills. During pregnancy, many autistic parents advocate effectively for accommodations and assert their preferences in healthcare settings, ensuring their needs are met (Hampton et al., 2022). These advocacy skills extend into parenting, where autistic parents champion their child’s rights and needs within educational, healthcare, and social systems.
Autistic mothers frequently demonstrate an ability to adapt to challenges while maintaining a strong sense of self and purpose, reflecting personal growth and empowerment through motherhood.
Empathy and Emotional Insight
Contrary to stereotypes that autistic individuals lack empathy, research highlights their capacity for profound emotional insight and connection. Many autistic parents report experiencing intense love and a unique bond with their children, driven by their shared neurodivergent experiences (Dugdale et al., 2021). This emotional depth fosters a parenting style rooted in understanding and acceptance, particularly when raising neurodiverse children.
Celebrating Neurodiversity in Parenthood
Highlighting and supporting these strengths is critical for creating a neuro-affirming maternity care experience. By reframing challenges as unique attributes and celebrating the diversity of parenting styles, maternity care providers can empower autistic parents to thrive during pregnancy and beyond. Integrating strengths-based approaches into parenting support frameworks can also help challenge stereotypes and foster a more inclusive understanding of autistic parenthood.
Quick Reference Guide for Professionals: Supporting Autistic Individuals During Pregnancy and Parenthood
Key Considerations
- Communication
- Use clear, direct, and unambiguous language.
- Provide written summaries, visual aids, and step-by-step explanations.
- Check for understanding without relying on outward affect, as it may not reflect internal comprehension.
- Sensory Needs
- Adjust clinical environments to be sensory-friendly (e.g., dim lights, reduce noise).
- Offer tools such as noise-cancelling headphones or weighted blankets.
- Allow for sensory breaks during appointments and labour.
- Continuity of Care
- Aim for consistent care teams to build trust and reduce anxiety.
- Provide detailed care plans for seamless handovers between providers.
- Mental Health
- Screen for prenatal and postnatal depression, anxiety, and PTSD.
- Provide access to autism-informed counselling and peer support groups.
- Inclusive Practices
- Use gender-affirming language and respect self-identified pronouns.
- Adapt care protocols to be culturally sensitive and neurodiverse-inclusive.
- Strength-Based Approaches
- Celebrate the unique strengths of autistic parents, such as systemising, planning, and sensory attunement.
- Reframe challenges as differences, not deficits, to foster empowerment.
Practical Strategies
- Appointment Adjustments:
- Extend appointment times to allow for detailed discussions and processing.
- Schedule quieter, low-traffic appointment slots when possible.
- Sensory Checklists:
- Provide a pre-appointment checklist for patients to identify their sensory needs and triggers.
- Training:
- Implement autism-specific training for maternity care providers, led by autistic individuals where possible.
- Support Networks:
- Facilitate connections to peer-led support groups and community resources for autistic parents.
- Feedback Mechanisms:
- Create safe channels for autistic patients to provide feedback on their care experiences.
Key Reminders for Professionals
- Affect Does Not Equal Understanding:
- An autistic individual may appear calm or engaged but could be overwhelmed or shutting down internally.
- Transitions Can Be Stressful:
- Clearly explain changes in care or procedures, and offer gradual transitions whenever possible.
- Stigma Persists:
- Avoid assumptions about parenting abilities and provide non-judgemental, tailored support.